Brain Stem Glioma
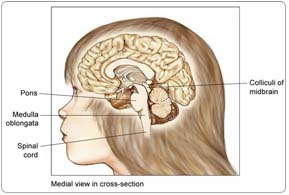
The brain stem connects the brain to the spinal cord. It is the lowest portion of the brain, above the back of the neck. The brain stem controls many of the body's basic functions, such as motor and sensory activity, coordination and walking, and heart and respiratory functions. It has three parts:
- The midbrain, which develops from the middle of the brain
- The medulla oblongata, which connects to the spinal cord
- The pons, which is located between the medulla oblongata and the midbrain
 Most brain stem tumors develop in the pons. A glioma is a tumor that grows from a glial cell, which is a supportive cell in the brain.
Most brain stem tumors develop in the pons. A glioma is a tumor that grows from a glial cell, which is a supportive cell in the brain.
Brain stem glioma is most often diffused (spread freely) through the brain stem by the time of diagnosis. This type of tumor is very aggressive. A small percentage of brain stem tumors are very localized or focal tumors. Focal tumors often are low-grade (the cells look close to normal) tumors, and behave in a more benign (less aggressive) fashion.
Brain stem glioma tends to occur in children between five and 10 years old. Most tumors grow in a part of the brain stem that can be difficult to perform surgery in, making brain stem glioma challenging to treat.
Risk Factors
A risk factor is anything that increases a person's chance of developing a disease, including cancer. There are risk factors that can be controlled, such as smoking, and risk factors that cannot be controlled, such as age and family history. Although risk factors can influence disease, for many risk factors it is not known whether they actually cause the disease directly. Some people with several risk factors never develop the disease, while others with no known risk factors do.
Doctors and researchers don't know what causes most childhood cancers. Some evidence indicates that genetic factors may play a role in a small percentage of brain stem gliomas. Genetic conditions associated with a higher risk of central nervous system (CNS) tumors include Li-Fraumeni syndrome, tuberous sclerosis, nevoid basal cell syndrome, and Turcot syndrome.
Symptoms
Children with brain stem glioma often experience the following symptoms. Sometimes, children with brain stem glioma do not show any of these symptoms. Or, these symptoms may be similar to symptoms of other medical conditions. If you are concerned about a symptom on this list, please talk to your child's doctor.
- Double vision or an inability to close the eyelids
- Drooping of the face
- Difficulty chewing and swallowing food
- Weakness in the arms and legs, clumsiness or wobbliness, and difficulty walking
- Difficulty talking
- Headache
- Vomiting
Diagnosis
Doctors use many tests to diagnose cancer and determine if it has metastasized (spread). Some tests may also determine which treatments may be the most effective. For most types of cancer, a biopsy is the only way to make a definitive diagnosis of cancer. However, biopsies are rarely used and are often specifically avoided in children with diffuse brain stem glioma because they do not influence treatment, and they can carry major risks. In addition, the diagnosis can generally be made by magnetic resonance imaging (MRI) alone (see below). Diffuse brain stem glioma is unlike most other types of tumors in this regard. For a focal tumor, a biopsy and surgical tumor removal may be considered. If a biopsy is not deemed possible, the doctor may suggest other tests that will help make a diagnosis. Imaging tests may be used to find out whether the cancer has metastasized. Your child's doctor may consider these factors when choosing a diagnostic test:
- Age and medical condition
- The type of cancer
- Severity of symptoms
- Previous test results
The following tests may be used to diagnose brain stem glioma:
Physical examination. A physical examination may include tests to determine brain function, reflexes, vision, and hearing of the child.
Computed tomography (CT or CAT) scan. A CT scan creates a three-dimensional picture of the inside of the child's body with an x-ray machine. A computer then combines these images into a detailed, cross-sectional view that shows any abnormalities or tumors. Sometimes, a contrast medium (a special dye) is injected into a vein to provide better detail. For a brain stem tumor, this test is generally insufficient to establish the diagnosis conclusively, and an MRI is required (see below).
Magnetic resonance imaging (MRI). An MRI uses magnetic fields, not x-rays, to produce detailed images of the body.
Biopsy. A biopsy is not generally done for the more common diffuse types of brain stem tumors. However, for focal tumors, it is often used to determine the type of cancer. If possible, a neurosurgeon (a specialist who operates on the head and brain) will remove a small piece of tissue from the brain. The doctor will examine the tissue under a microscope and look for cancer cells.
Treatment
Clinical trials are the standard of care for the treatment of children with cancer. In fact, more than 60% of children with cancer are treated as part of a clinical trial. Clinical trials are research studies that compare standard treatments (the best treatments available) with newer treatments that may be more effective. Cancer in children is rare, so it can be hard for doctors to plan treatments unless they know what has been most effective in other children. Investigating new treatments involves careful monitoring using scientific methods, and all participants are followed closely to track progress.
To take advantage of these newer treatments, all children with cancer should be treated at a specialized cancer center. Doctors at these centers have extensive experience in treating children with cancer and have access to the latest research. Many times, a team of doctors treats children with cancer. Pediatric cancer centers often have extra support services for children and their families, such as nutritionists, social workers, and counselors. Special activities for kids with cancer may also be available.
Three types of therapies can be used to treat brain stem glioma in children: radiation therapy, surgery, and chemotherapy. Sometimes, the treatments are used in combination.
Radiation therapy
Radiation therapy uses x-rays or other high-energy particles to kill cancer cells. Radiation therapy is the most common treatment for brain stem glioma.
Fatigue, drowsiness, nausea, vomiting, and headache are common side effects of radiation therapy. Because radiation therapy can sometimes interfere with the normal growth and development of the child's brain, the doctor may choose to treat the cancer in another way. To avoid or reduce the need for radiation treatment in young children, the doctor may use chemotherapy to shrink the tumor.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells. Because it kills cancer cells throughout the body, it is called a systemic treatment.
Chemotherapy alone is not an effective treatment for brain stem glioma; however, in some cases, a doctor may use chemotherapy during or after radiation treatments.
Because chemotherapy attacks rapidly dividing cells, including those in normal tissues such as the hair, lining of the mouth, intestines, and bone marrow, children receiving chemotherapy may lose their hair, develop mouth sores, or have nausea and vomiting. Chemotherapy may lower the body's resistance to infection, lead to increased bruising and bleeding, and cause fatigue. These side effects can be controlled during treatment and usually go away after chemotherapy is completed. The severity of the side effects depends on the type and amount of the drug being given and the length of time the child receives the drug.
The medications used to treat cancer are continually being evaluated. Talking with your doctor is often the best way to learn about the medications you've been prescribed, their purpose, and their potential side effects or interactions with other medications. Learn more about your prescriptions through PLWC's Drug Information Resources, which provides links to searchable drug databases.
Surgery
Surgery is used to treat brain stem glioma only when the tumor's appearance on an MRI scan is focal, thus suggesting it may be possible to remove the cancer without damaging the brain, such as when a tumor grows out from the brain stem. For most children with diffuse types of brain stem gliomas, surgery is not necessary or possible because of the location of the tumor and the risk involved.
Recurrent brain stem glioma
Treatment for recurrent brain stem glioma (cancer that comes back after treatment) depends on two factors:
- The type of tumor
- The type of treatment the child received for the original tumor
Depending on individual circumstances, the doctor may recommend either surgery or chemotherapy.
Side Effects of Cancer and Cancer Treatment
Cancer and cancer treatment can cause a variety of side effects; some are easily controlled and others require specialized care. Below are some of the side effects that are more common to brain stem glioma and its treatments. For more detailed information on managing these and other side effects of cancer and cancer treatment, visit the PLWC Managing Side Effects section.
Anemia. Anemia is common in people with cancer, especially those receiving chemotherapy. Anemia is an abnormally low level of red blood cells (RBCs). RBCs contain hemoglobin (an iron protein) that carries oxygen to all parts of the body. If the level of RBCs is too low, parts of the body do not get enough oxygen and cannot work properly. Most people with anemia feel tired or weak. The fatigue (tiredness) associated with anemia can seriously affect quality of life and make it more difficult for patients to cope with cancer and treatment side effects.
Fatigue. Fatigue is extreme exhaustion or tiredness, and is the most common problem that people with cancer experience. More than half of patients experience fatigue during chemotherapy or radiation therapy, and up to 70% of patients with advanced cancer experience fatigue. Patients who feel fatigue often say that even a small effort, such as walking across a room, can seem like too much. Fatigue can seriously impact family and other daily activities, can make patients avoid or skip cancer treatments, and may even impact the will to live.
Hair loss (alopecia). A potential side effect of radiation therapy and chemotherapy is hair loss. Radiation therapy and chemotherapy cause hair loss by damaging the hair follicles responsible for hair growth. Hair loss may occur throughout the body, including the head, face, arms, legs, underarms, and pubic area. The hair may fall out entirely, gradually, or in sections. In some cases, the hair will simply thin-sometimes unnoticeably-and may become duller and dryer. Losing one's hair can be a psychologically and emotionally challenging experience and can affect a patient's self-image and quality of life. However, the hair loss is usually temporary, and the hair often grows back.
Mouth sores (mucositis). Mucositis is an inflammation of the inside of the mouth and throat, leading to painful ulcers and mouth sores. It occurs in up to 40% of patients receiving chemotherapy treatments. Mucositis can be caused by a chemotherapeutic drug directly, the reduced immunity brought on by chemotherapy, or radiation treatment to the head and neck area.
Nausea and vomiting. Vomiting, also called emesis or throwing up, is the act of expelling the contents of the stomach through the mouth. It is a natural way for the body to rid itself of harmful substances. Nausea is the urge to vomit. Nausea and vomiting are common in patients receiving chemotherapy for cancer and in some patients receiving radiation therapy. Many patients with cancer say they fear nausea and vomiting more than any other side effects of treatment. When it is minor and treated quickly, nausea and vomiting can be quite uncomfortable but cause no serious problems. Persistent vomiting can cause dehydration, electrolyte imbalance, weight loss, depression, and avoidance of chemotherapy.
Nervous system disturbances. Nervous system disturbances can be caused by many different factors, including cancer, cancer treatments, medications, or other disorders. Symptoms that result from a disruption or damage to the nerves caused by cancer treatment (such as surgery, radiation treatment, or chemotherapy) can appear soon after treatment or many years later. See Managing Side Effects: Nervous System Disturbances for the most common symptoms.
Sleeping problems: hypersomnia, somnolence syndrome, and nightmares. Hypersomnia, also called somnolence, excessive daytime sleepiness, or prolonged drowsiness, is a condition characterized by excessive sleeping or the inability to maintain wakefulness when desired. Somnolence syndrome is a type of hypersomnia associated with cranial radiation therapy (radiation treatment to the head) in children. Symptoms of somnolence syndrome include excessive drowsiness, prolonged periods of sleep (up to 20 hours a day), headaches, low-grade fever, nausea and/or vomiting, and irritability. Nightmares are vivid, frightening dreams that usually cause the dreamer to wake up able to remember part or most of the nightmare. Most people have nightmares from time to time, but the frequency or vividness of nightmares can increase after a cancer diagnosis and during cancer treatment. Possible causes of hypersomnia include some brain cancers in adults (for example, ependymoma or meningioma); some childhood central nervous system (CNS) cancers (for example, brain stem glioma, cerebellar astrocytoma, medulloblastoma); some secondary brain tumors (brain metastases); some chemotherapeutic drugs (for example, teniposide [VM-26], pegaspargase [Oncaspar], thalidomide [Thalomid]); and other prescription and over-the-counter medications (for example, some antidepressants, antinausea medications, opioid pain killers, sedatives, antihistamines, sleeping pills).
After Treatment
The child's follow-up care plan and the long-term risks following therapy depend on several factors, such as the type of tumor and its location, the age of the child, and the type of treatment. For example, craniospinal radiation therapy can cause cognitive and endocrine symptoms over time, although the severity can vary greatly depending on the dose administered and the age of the child. Similarly, the risks and potential side effects of surgery vary dramatically, depending on the location and characteristics of the tumor. Likewise, the risks of chemotherapy and the likelihood of secondary cancers are strongly influenced by the drugs used and their doses. For each of these issues, it is important to discuss the specific aspects of the tumor and the options for treatment with the neurosurgeons and neuro-oncologists that are involved in the child's care.