What is it?
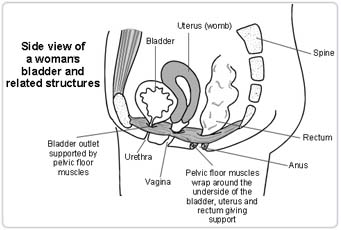
The vagina and the back passage - rectum are no longer held up properly. The rectum is dropping down onto the back of the vagina, making a weakness or bulge. The bulge is called a prolapse. A prolapsed rectum is called a rectocele. The prolapsed rectum may not empty properly when you want. The prolapse makes you feel uncomfortable in the vagina. The prolapse happens if the supports to the vagina and rectum stretch during pregnancy, and do not get back to normal afterwards. This may not show up until after the menopause. Having a heavy job, having a chronic cough, or being overweight will all bring on a prolapse earlier. An operation will tighten up the supports to the rectum, and take away the bulge in the vagina.
The Operation
You will have a general anaesthetic and be completely asleep. A small cut is made through the lining of the back - posterior of the vagina. The supports to the rectum are shortened with stitches and the bulging part of the vagina cut away. This repairs the weakness. The wound in the vagina is then stitched up. You need to be in hospital for about six days.
Any Alternatives
If you leave things as they are, the prolapse will slowly get bigger. Your discomfort and difficulty opening the bowels will worsen. The bulge may even drop through the vulva and start to bleed. At your stage, special exercise to the muscles of the pelvis have not helped. A prolapse is not a serious/life-threatening condition but it can seriously affect the quality of your life. . Your best way forward is to have the operation. The operation is relatively easy to perform and is successful most of the time.
Before the operation
Stop smoking and get your weight down if you are overweight. (See Healthy Living). If you know that you have problems with your blood pressure, your heart, or your lungs, ask your family doctor to check that these are under control. If you are past the menopause, your vagina may be short of female hormone (oestrogen). You may heal better if you have some hormone replacement treatment (HRT). You may be started on this before your operation using tablets, patches, or a vaginal cream. This will be for a month or two to cover the operation only. You don't need to decide at this stage about having long-term HRT. Check that you have a relative or friend who can come with you to the hospital, take you home, and look after you for the first week after the operation. Sort out any tablets, medicines, inhalers that you are using. Keep them in their original boxes and packets. Bring them to hospital with you. On the ward, you may be checked for past illnesses and may have special tests to prepare you so that you can have the operation as safely as possible. . Please tell the doctors and the nurses of any allergies to tablets, medicines or dressings. You will have the operation explained to you and will be asked to fill in an operation consent form. Many hospitals now run special preadmission clinics, where you visit for an hour or two, a few weeks or so before the operation for these checks.
After - In Hospital
You will have a small/thin plastic tube (a drip) in an arm vein. This gives you salt and sugar and water, and sometimes blood, for a day or so from a plastic bag on a stand. You may be given oxygen from a face mask for a few hours if you have had chest problems in the past. You will have a sanitary pad in place. The wound may be painful. You will be given painkilling injections or tablets for this. On the second day you should be able to spend an hour or two out of bed. By the end of four days you should have little pain. A general anaesthetic will make you slow, clumsy and forgetful for about 24 hours. Do not make important decisions during that time. The nurses will help you with everything you need until you can do things for yourself.
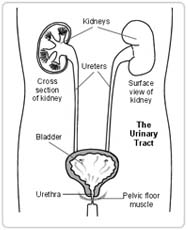
You will have some blood and urine tests in the first few days after your operation. These will check you are not anaemic and have no infection in the urine. You may have a fine tube - catheter in the your bladder . This drains urine from your bladder into a collection bag at your bedside. It is usually taken out two days after your operation. You will then pass urine normally. The catheter will makes you feel as though you need to pass urine. This is a false alarm. If you do not have a catheter, you need to pass urine within six hours after the operation. If you have any difficulty, tell the nurses. There are stitches in the skin wound in the vagina. The parts of the stitches under the skin will melt away by themselves. The surface knots of the stitches will appear on the pads after about two weeks. This is quite normal. You should wear pads as dressings. Do not use tampons for six weeks. There will be slight bleeding like the end of a period. It should be almost nil by the time you leave the hospital. There may be a little bleeding again after about two weeks when the knots free off. This is nothing to worry about. If it is heavy, contact the ward.
You will be able to take a bath or shower as often as you wish. You do not need salt water. Do not soak in the bath for more than 10 minutes. Gently dry the wound area afterwards. You will be given an appointment for an Out Patient check up about six weeks after you leave hospital. The nurses will advise about sick notes, certificates etc.
After - At Home
At home, you are likely to feel tired and need rest two or three times a day for a for three to four weeks. You will gradually improve. After three months, you should be able to return completely to your usual level of activity. You can drive as soon as you can make an emergency stop without discomfort, generally after three weeks. You can start sexual relations before you return for the six-week check, if you feel comfortable enough, and you have no blood loss. You should be able to return to a light job after about six weeks. Leave a very heavy or busy job until 12 weeks.
Possible Complications
As with any operation under general anaesthetic there is a very small risk for complications related to your heart or your lungs. The tests that you will have before the operation will make sure that you can have the operation in the safest possible way and will bring the risk for such complications very close to zero.
Most vaginal repairs are without complication. Problems are being looked for by the medical and nursing staff. If you think that all is not well, please ask the nurses or doctors.
Minor complications occur in 3-4% of cases. Chest infections may arise, particularly in smokers. Work with the physiotherapists to clear the air passages to prevent this. Do not smoke. Sometimes the bladder is slow to start working again. Be patient. Sometimes the catheter needs to go back into the bladder for a few days. Wound infection is sometimes seen. This settles down with antibiotics in a week or two. Aches and twinges may be felt in the vaginal area for up to three months.
More serious complications such as severe bleeding, damage to your bowel by the operation, or a creation of a passage between your vagina and the bowel (fistula) are rare (1-2% of cases) and may require another operation to fix them.
Advanced Reproductive Technology
- In Vitro Fertilisation (IVF)
- Intracytoplasmic Sperm Injection (ICSI)
- Donor egg and embryo programs
- In Vitro Fertilisation (IVF)
- Pre-implantation genetic diagnosis (PGD)
- Surrogacy programs
Dental Videos